Lawrence G. Kass, M.D., The Center for Cosmetic Facial & Eye Plastic Surgery
6025 4th Street North St. Petersburg, Florida 33703
LHE was initially branded as IPL (intense pulsed light) or even soft laser it was a brand new technology using light and heat energy to treat skin imperfections. LHE was designed to reduce the risk of injury while providing the same results as lasers or IPL. LHE Photo-rejuvenation takes just ten minutes with NO preparation. This is a big difference as lasers and IPL requires the use of gel or contact cooling. LHE promises no downtime which gives client's the opportunity to squeeze in a lunch hour appointment and still have plenty of time for lunch. Noticeable improvement in pigmentation, facial veins, red blotches, and fine lines and wrinkles occur after just a few treatments.Using the advanced LHE technology, precise amounts of light energy is delivered to the skin's surface. Treatments are spaced at three week intervals. The energy is delivered at specific settings for each treatment to maximize your results.
Rejuvenation is designed to combat the effects of aging and damaged skin in a softer, gentler way. The advanced LHE technology can remove 90-95% of pigmented spots effectively. The redness and flushing of rosacea can be reduced 80-90%. The light energy stimulates the production of collagen, reducing pore size, fine lines, and wrinkles. It can be used to treat the full face, neck, chest and even the hands and is also effective in treating acne.
See Clinical Descriptions of Selected Patients in Photo Galleries
The best candidates for photofacial rejuvenation have red, flushed faces, unsightly facial veins, sun-damaged skin, hyperpigmentation, or enlarged pores.
Tuesday, October 30, 2012
LHE PhotoFacial Rejuvenation
LHE Skin Photorejuvenation
Lawrence G. Kass, M.D., The Center for Cosmetic Facial & Eye Plastic Surgery
6025 4th Street North St. Petersburg, Florida 33703
Wrinkles, age spots, sun spots and spider veins – medically known as rhytides and pigmented and vascular lesions, are outward manifestations of aging or sun damaged skin. Once accepted as a fact of growing older, these skin imperfections can now be safely and easily treated.A comprehensive skin rejuvenation treatment may include several treatment goals simultaneously; the improvement of fine lines and skin texture and the removal of age spots and spider veins. LHE has demonstrated a clinically proven ability to safely deliver more youthful looking skin and a high level of client satisfaction. Another term often used to describe LHE is photofacial rejuvenation. LHE technology's innovative balance of Light and Heat creates a more efficient photothermal process that enables low energy levels. This low energy level (measured in Joules/cm²) optimizes safety and eliminates the need for pre-treatment protocols or skin cooling techniques. Non ablative, LHE treatments are faster and safer with absolutely no downtime, giving your clients the freedom to squeeze a quick appointment into their busy day.
How LHE Photorejuvenation Works
As skin ages and is exposed to the elements of nature, it suffers from degradation and imperfections. Using LHE technology, short pulses of light and heat selectively target and coagulate chromophores in the epidermis and papillary dermis. Oxy-hemoglobin in vascular lesions and melanin in pigmented lesions are coagulated. The coagulated cells are eliminated by a natural process and replaced by new cells. At the same time, LHE creates a mild thermal insult to the dermal-epidermal junction. The insult triggers a wound-healing process and new collagen remodels under an undamaged outer layer. As collagen rebuilds, fine lines and wrinkles disappear or fade. LHE results in clearer, smoother, younger looking skin. The best candidates for LHE rejuvenation have red, flushed faces, unsightly facial veins, sun-damaged skin, hyperpigmentation, or enlarged pores.
LHE Skin Photorejuvenation is Non-Ablative Photo Rejuvenation technology. The treatments are Fast and very importantly No Downtime.
Lawrence G. Kass, M.D., The Center for Cosmetic Facial & Eye Plastic Surgery
6025 4th Street North St. Petersburg, Florida 33703
http://www.kassmd.com/psoriasis-treatment.html
Psoriasis affects 100 million people worldwide. With 150,000 – 200,000 new cases being diagnosed in the United States each year. Its annual cost to society is over 3 billion dollars in the U.S. alone. It is a disease of the immune system whose causes are still largely unknown. Psoriasis is cyclical in nature. Patients experience episodes of flare-ups alternated with periods of remission that come and go over a lifetime. Although the onset of psoriasis can occur at any age, most cases appear between ages 15-35. Far more than just a “simple skin disease”, psoriasis is a chronic, debilitating and often painful condition. Skin regenerates approximately 10 times faster than normal, creating a white flakey buildup over a patch of red inflamed skin. Psoriasis is characterized by dry, rough and scaly skin that constantly flakes and peels as well as almost unremmittent itching and burning. Even in its mildest forms psoriasis can make life miserable. And the costs of psoriasis cannot always be measured in money spent. Visible psoriatic lesions can have a negative impact on careers and social life and a psoriasis patient often feels cut off, abandoned and hopeless. Although rarely life threatening, recent studies have shown that psoriasis sufferers rate their quality of life at a level lower than those of diseases usually considered much more serious such as arthritis, diabetes, and cancer.
LHE Phototherapy for Psoriasis Halts the Cycle
LHE provides relief without the need for topical therapies, oral medications, painful injections or exposure to potentially cancer-causing ultraviolet light. LHE psoriasis phototherapy for mild to moderate chronic plaque and guttate psoriasis is a revolutionary and powerful tool in the never-ending battle against psoriasis. A completely safe and painless light-based therapy, LHE can bring complete relief from itching in as little as 2 – 3 sessions. Most patients experience a 75% clearance in psoriatic lesions after a full treatment course of 8-10 sessions carried out over 4-5 weeks.
How LHE for Psoriasis Works
In normal skin, the cells grow, move to the surface and are sloughed off at a steady unnoticeable rate. This cycle takes about one month. With psoriasis, the immune system sends faulty signals that speed up this cycle to only three or four days. The skin thickens with extra cells and blood vessels grow larger in a attempt to feed those extra cells. Skin cells pile up on the surface with dead cells creating a white, flaky layer over the patch of inflamed skin. LHE uses specialized flashes of green and yellow Light to shrink and eliminate the blood vessels that feed the abnormal growth of psoriatic skin cells. The Heat combined with infrared wavelengths reduce swelling and inflammation and very effectively stop the constant itching associated with psoriasis. Although psoriasis can occur on many areas of the body, LHE’s selective photothermolysis treatments insure that only psoriatic lesions are treated while healthy tissue remains untouched.
Treatment of psoriasis with light and heat energy xLHE
Drs. A Leviav, R Wolf, and A Vilan
Dermatology Online Journal 10 (2): 4
Abstract
In psoriasis the earliest observable electron microscopic changes are in the papillary dermis vasculature. Selective photothermolysis of the dermal vasculature using a 585-nm pulsed-dye laser (PDL) for the treatment of psoriasis was reported more than a decade ago. Although clinically effective, the pulsed-dye laser has limited practicality because of small spot size (5-10 mm) and lack of cost effectiveness. The objective of this study is to evaluate the safety and efficacy of a novel Light and Heat Energy (LHE™) selective-photothermolysis system for the treatment of psoriasis. This system delivers controlled heat simultaneously with the light pulse; it has a large beam spot (55 × 22 mm) and is sufficiently cost effective to be widely used. Thirteen patients, seven with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis participated in a controlled study. Patients received two therapy regimens in parallel: LHE™ plus salicylic acid or salicylic-acid cream alone as control. Treatments were applied twice weekly spread evenly over 4-6 weeks. In most cases a fluence of 8.6 J/cm² was applied. Efficacy of the treatment was assessed using the psoriasis-severity index (PSI) calculated from the investigator's overall assessment of the plaque's erythema, scaling, and induration. PSI was evaluated at baseline, at every other treatment visit, and during two follow-up visits scheduled 1 and 5 weeks following the last treatment.
In eleven patients who completed the treatment regimen, the average global PSI score for the treated sites was reduced by 65 percent. In contrast, the control sites average global PSI score was reduced by only 7.4 percent. Six patients (55 %) had a significant improvement of 70-percent reduction or above in their PSI score, ten patients (91 %) had a 50 percent or above reduction; only one patient had a poor response (12.5 % reduction in global PSI). Erythema was reported in all cases and resolved within 24-48 hours. Six cases of burns were resolved within 2 days to 2 weeks following appropriate remedy. No cases of dyspigmentation were encountered.
Light and Heat Energy (LHE™) selective photothermolysis combined with salicylic acid appears to be a practical modality for the treatment of mild to moderate psoriasis. Patients experience discomfort that is only mild. There is no convalescence downtime. Clinical results obtained are similar to those reported with the pulsed-dye laser; however, this new system seems more suitable to be widely adopted as a treatment modality. Further followup is required to determine whether remission periods will be as long as those reported for treatment with the pulsed-dye laser.
Introduction
In psoriasis, the earliest observable electron-microscopic changes are in the papillary dermal vasculature. These vessels have been implicated as participating in the pathogenesis of the disease by facilitating the access of activated T cells to the skin and maintaining the psoriatic plaque [1, 2]. Treatment of psoriasis by selective photothermolysis of the dermal vasculature using a 585-nm pulsed-dye laser (PDL) has been suggested; several studies on the use of this laser to treat psoriasis have been published [3, 4, 5, 6, 7, 8]. Ros et al. [5] found a beneficial clinical effect on six of ten patients treated with PDL. The psoriasis-severity score in these patients was reduced to 2.2 ± 1.3, compared with 7.2 ± 1.7 for control areas (69 % reduction). Plaques readily developed crusting in which the necrotic former epidermis was apparent. Zelickson et al. [6] found significant clinical improvement in chronic plaque-type disease using both short (0.45 ms) and long (1.5 ms) pulsed-dye laser. Patients responding to treatment remained in remission for up to 13 months. A more recent followup found that some of the patients are still clear of the disease 5-6 years out. One patient showed no recurrence 7 years after PDL treatment. Although clinically effective, pulsed-dye laser has limited practicality because of a small (5-10 mm) spot size and lack of cost effectiveness.
The Radiancy Light and Heat Energy (LHE™) system is a new, potentially more effective selective-photothermolysis system for the treatment of psoriasis. In addition to green and yellow light for the coagulation of the psoriatic capillaries, this nonlaser system also emits a pulse of heat, which reduces swelling and inflammation and relieves pruritus [9, 10]. Using a broadband flashlamp, this small, tabletop device delivers a light energy fluence of 4-10 J/cm² with a beam spot of 55 × 22 mm, enabling rapid coverage of large lesion areas.
Methodology and treatment
A study was undertaken to assess the safety and efficacy of this LHE™ system in the treatment of patients with psoriasis. The study was designed as an intrapatient controlled study comparing the efficacy of two therapies for psoriasis given in parallel: LHE™ plus 20 percent salicylic acid (SCA) and 20 percent salicylic acid alone. The study was jointly conducted by the departments of plastic surgery and dermatology, Kaplan Hospital, Israel, following approval of the Helsinki Committee. Thirteen patients were enrolled in the study, seven with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis. Patients received two therapy regimens in parallel: ten biweekly treatments of LHE plus salicylic acid for a total of 5 weeks or salicylic-acid cream alone for the same time duration. In both regimens patients were asked to apply SCA daily except during treatment days. Treatment areas were a single (unilateral) plaque or double (bilateral), symmetrical plaques. In case of bilateral lesions, the right side was treated with LHE plus SCA; the left side was treated with SCA alone. In case of a unilateral lesion, the upper segment was treated with LHE plus SCA; the lower segment was treated with SCA alone.
Photographs of the psoriatic lesions were taken at baseline, at every other treatment visit, and during the first and second follow-up visits, conducted at 1 and 5 weeks following the last treatment.
Efficacy of the treatment was assessed using the Psoriasis Severity Index (PSI) calculated from the investigator's overall assessment of the plaque erythema, scaling, and induration. Score was defined as 0 = absent; 1 = minimal, light pink, rare scale, barely perceptible elevation; 2 = mild light red/pink, poorly defined scale, light elevation; 3 = moderate red, defined scales, moderate elevation; 4 = severe. very red, heavy scales, marked ridge. Global PSI score was calculated as the sum of erythema, scaling, and induration scores. PSI was evaluated at baseline, at every other treatment visit and during the first and second follow-up visits. The investigator performing the assessment was not blinded to treatment.
A total of thirteen patients with psoriasis were enrolled to the study in accordance with the following criteria:
- The patient is at least 18-years old.
- The patient has clinically diagnosed mild to moderate psoriasis (at least 10 % body area).
- Psoriasis is relatively symmetric and homogeneous.
- The patient is not on any other treatment.
- The patient is capable of reading, following instructions, and understanding the procedure to be applied.
- The patient is committed to all treatment and follow-up visits.
The patients were excluded according to the following criteria:
- The patient has used topical or systemic antipsoriatic therapy within 3 weeks prior to the start of the study.
- The patient has a history of carcinoma of the skin.
- The patient has used of any medication that can cause photosensitivity or affect integrity of the skin.
- The patient has had sun exposure or artificial tanning in the treatment area 2-weeks prior to study enrollment.
- The patient has a history of photosensitivity or intolerance to ultraviolet radiation.
The patient has a history of hypertrophic scar or keloid formation.
- The patient has a history of pigmentary changes in areas of trauma or burn.
- The patient has existing skin diseases other than psoriasis.
- The patient is pregnant
- The patient has epilepsy.
Before enrollment each patient completed a medical history form and signed an informed consent form. Three patients did not complete the treatment and followup for various reasons: One dropped out after the first visit, another after the third treatment, and the third completed treatments but did not appear for the follow-up visits. Mean age of the patients was 53.6 ± 6.4 years (range 44-67). Ten patients were females and three males. Six patients were Fitzpatrick skin types II (5 female, 1 male), five patients were skin types III (4 female, 1 male), and two were skin types V (1 female, 1 male).
Seven patients were diagnosed with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis. Three patients were treated on the elbow, two on the knee, one on the palm, five on the foot, three on the leg, and three on the arm.
Patients were instructed to clean the area thoroughly with soap and water and ensure that the skin surface is dry before treatment. On the basis of a pretreatment test conducted 48-72 hours prior, the highest power level that caused redness and erythema without blisters was used for treatment. Pulses were administered sequentially on the treatment area from right to left with no more than 20 percent overlap. After covering the entire area the investigator waited 5 minutes to allow the skin to cool, and repeated the procedure once more. For small lesions, a small-area adaptor was used. In this case fluence was increased by 10 percent to compensate for light scatter. Treatments were applied twice weekly spread evenly over a 4-6 week period. When no results were seen after 3 treatments, fluence was increased by 10 percent.
In most cases a fluence of 8.6 J/cm² was found to be the most effective and safe treatment parameter.
Results
Plaque assessment on the treated site (LHE plus SCA) and the control site (SCA alone) was conducted by the investigator at baseline, prior to any treatment, at each odd-numbered treatment visit and at the two follow-up visits. Of the eleven patients who completed the treatment regimen, one underwent a total of 8 treatments, three a total of 10 treatments, three a total of 11 treatments, and four a total of 12 treatments.
Figure 1
Average global PSI at different stages of treatment.
Average global PSI score at baseline for the treated sites (LHE plus SCA) was 8.36 (range 6-11). This was reduced by 65 percent to 2.91 (range 0-7) at the final visit. Scaling score in these sites was reduced from an average of 2.82 to 1.00 (64 % reduction); erythema score was reduced from 2.64 to 1.00 (62 %); and induration score was reduced from 2.91 to 0.91 (69 %). Nine patients appeared for the first follow-up visit (FU1), and only seven for the second follow-up visit (FU2). In this latter group, average global PSI score further reduced to 2.57 (69 %) possibly indicating the effect of the final treatment. The reduction in global PSI score, over the treatment course, for the lesions treated with LHE plus SCA is shown in Fig. 1.
Of the eleven patients who completed the treatment regimen only one had a poor response (12.5 % reduction in global PSI). Ten of the patients (91 %) had a 50 percent or above reduction in their PSI score, and six patients (55 %) had a significant improvement of 70 percent reduction or above.
In contrast, on the control sites (SCA alone) average global PSI score at baseline was 7.71 (range 4-10), and this score was reduced by only 7.4 percent to an average of 7.14 (range 3-9). Scaling was reduced by 5.2 percent, erythema by 5.8 percent, and induration by 10.9 percent.
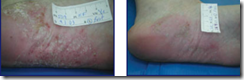
Figure 2a
Figure 2b
Before treatment (Fig. 2). After treatment (Fig. 2a).
Figure 3a
Figure 3b
Before treatment (Fig. 3). After treatment (Fig. 3a).
Figure 4a
Figure 4b
Before treatment (Fig. 4). After treatment (Fig. 4a).
Figure 5a
Figure 5b
Before treatment (Fig. 5). After treatment (Fig. 5a).
The safety of the LHE psoriasis treatment was determined by clinical observation and evaluation of the treated areas. Potential adverse clinical effects, such as erythema, crusting, blistering, scars, and hyper- or hypopigmentation, were evaluated by the investigator in each treated area immediately after treatment, between treatments, and during the follow-up visits. Erythema was reported in all cases and resolved within 24-48 hours. Six cases of burns (five with blistering) were reported; these patients were given appropriate remedy (Silverol or Biafine) and the reaction resolved within 2 days to 2 weeks. No cases of dyspigmentation were encountered.
Conclusions
Radiancy's Light and Heat Energy (LHE™) selective-photothermolysis system, combined with salicylic acid, appears to be an effective modality for the treatment of mild to moderate psoriasis. In most cases (6/10) a significant reduction of over 70 percent in global PSI score was achieved. In almost all cases (10/11) at least a moderate improvement (greater than 50 %) was obtained; only one case resulted in insignificant (12.5 % reduction) response. Overall, average global PSI score for the eleven patients who completed the treatment regimen was reduced by 65 percent from 8.36 to 2.91. In contrast, control treatment of salicylic acid alone resulted in an average global PSI score reduction of only 7.4 percent. No improvement occurred in 71 percent of the control lesions, and 29 percent exhibited very modest improvement.
Side effects were mild and transient with resolution at 2 weeks post-treatment at most. The only discomfort patients experienced was mild. There was no downtime for convalescence.
The clinical results obtained with the Radiancy LHE™ system in the treatment of psoriasis are remarkably similar to those reported with the pulsed-dye laser. In contrast to pulsed-dye laser, the LHE system is compact, simple to operate, and cost effective; we consider this form of treatment to be highly suitable to be widely adopted as a treatment modality for mild to moderate psoriasis. Further followup is required to determine whether remission periods will be as long as those reported for treatment with the pulsed-dye laser.
Conflict of Interest Statement: A Vilan is a medical consultant for Radiancy. Drs. Leviav and Wolf have no financial interest relating to this work.
References
1. Pinkus H, Mehregan AH. The primary histologic lesion of seborrhoic dermatitis and psoriasis. J Invest Dermatol. 46:109-116, 1966.2. Barker JN. The pathophysiology of psoriasis. Lancet. 1991 Jul 27;338(8761):227-30. PubMed
3. Hacker SM, Rasmussen JE. The effect of flash lamp-pulsed-dye laser on psoriasis. Arch Dermatol. 1992 Jun;128(6):853-5. PubMed
4. Katugampola GA, Rees AM, Laningan SW. Laser treatment of psoriasis. Br J Dermatol. 1995 Dec;133(6):909-13. PubMed
5. Ros AM, Garden JM, Bakus AD, Hedblad MA. Psoriasis response to the pulsed-dye laser. Lasers Surg Med. 1996;19(3):331-5. PubMed
6. Zelickson BD, Mehregan DA, Wendelschfer-Crabb G, Ruppman D, Cook A, O'Connell P, Kennedy WR. Clinical and histologic evaluation of psoriatic plaques treated with a flashlamp pulsed-dye laser. J Am Acad Dermatol. 1996 Jul;35(1):64-8. PubMed
7. Bjerring P, Zachariae H, Sogaard H. The flashlamp-pumped dye laser and dermabrasion in psoriasis--further studies on the reversed Kobner phenomenon. Acta Derm Venereol. 1997 Jan;77(1):59-61. PubMed
8. Hern S, Allen MH, Sousa AR, Harland CC, Barker JN, Levick JR, Mortimer PS. Immunohistochemical evaluation of psoriatic plaques following selective photothermolysis of the superficial capillaries. Br J Dermatol. 2001 Jul;145(1):45-53. PubMed
9. Orenberg EK, Noodleman FR, Koperski JA, Pounds D, Farber EM. Comparison of heat delivery systems for hyperthermia treatment of psoriasis. Int J Hyperthermia. 1986 Jul-Sep;2(3):231-41. PubMed
10. Boreham DR, Gasmann HC, Mitchel RE. Water bath hyperthermia is a simple therapy for psoriasis and also stimulates skin tanning in response to sunlight. Int J Hyperthermia. 1995 Nov-Dec;11(6):745-54. PubMed
Tuesday, October 23, 2012
Radiancy’s SHALS technology (Smart Heat Accumulation Light Sequence technology)
Radiancy’s SHALS Technology is patented and a revolutionary system that protects the epidermis while delivering the correct temperature in the dermis. SHALS is an acronym for Smart Heat Accumulation Light Sequence technology is design for uncompromised patient comfort and safety while ensuring great results. SHALS is used in Radiancy’s Mistral specifically for the skin tightening application. SHALS delivers the right heat into dermis causing a slight thermal insult to initiate collagen rebuilding. The end result will be a smooth supple skin and improved skin texture.
SHALS technology enables infrared light to penetrate deep into the lower dermal levels (1-2 mm) to set off a mild dermal trauma and initiate the wound/heal response. The collagen found in these levels responds with new growth, returning firmness and elasticity to the skin. As a result, fine lines and wrinkles become smoother and skin appears younger and fresher.
In order for this process to work properly, high temperatures in the deeper levels of the dermis are necessary. SHALS technology heats the deep dermal layers without bringing the outer layers of skin above the pain threshold of 42ºC.
SHALS, with proprietary algorithms that support a multi-pulse train, takes advantage of the difference in thermal relaxation times between the outer and inner layers of the skin. This enables the epidermis to remain cooler than the deeper dermal layers as they reach optimal treatment temperatures. A gentle lifting effect takes place, skin loses its laxity and wrinkles fade. Skin appears firmer, smoother and younger looking.
Radiancy’s SHALS技术是专利和革命性的系统,同时提供了正确的温度在真皮层和保护表皮。 SHALS是缩为写智能热积累光序列。它是同时确保伟大成果为不折不扣患者的舒适和安全设计。SHALS使用在Radiancy’s Mistral,专门为皮肤收紧应用程序。SHALS将正确的热传送到真皮造成轻微的热,导致胶原重建。最终的结果将是光滑柔软的皮肤和改善皮肤纹理。
SHALS技术使红外线光要深入到较低的真皮级别(1-2 毫米),以抵销轻度皮肤创伤和启动治愈伤口/响应。在这些级别中找到的胶原响应的新增长返回对皮肤的坚定性和弹性。其结果是,细纹及皱纹变得更平滑和皮肤出现更年轻、 更新鲜。
为了使这一进程能够正常工作,必要在深层的真皮层使用高温度。SHALS技术加热深真皮层,不会使外层的皮肤达到高过42ºC的痛阈。
SHALS,拥有支持多脉冲火车的专有算法,利用热弛豫时间在皮肤的外部和内部的图层之间的差异。这使表皮凉过深入真皮层,达到了最佳的治疗温度。这会造成温柔的提升效应发生、 皮肤失去其松弛和皱纹淡出。皮肤出现更稳固、 更平滑和年轻看。
Friday, October 19, 2012
CELHE (Center of Excellence Light Heat Energy)
What is CELHE?
CELHE (pronounced as Celia) is a dedicated group made for LHE practitioners in SE Asia.
Why CELHE?
There are pockets of LHE practitioners who have consistently produced phenomena results for the clients. This is a group where successful practitioners share tips on how they are able to produce phenomenal results.
Who can join CELHE?
CELHE is for all LHE practitioners.
How can I join CELHE?
You must be located either in Malaysia, Singapore or Indonesia. You can write to contact@lifvation.com for meeting schedules. Our first meeting will be on 19th November in Singapore.
What happens in the CELHE group?
Regular sharing session, training, workshops