Drs. A Leviav, R Wolf, and A Vilan
Dermatology Online Journal 10 (2): 4
Abstract
In psoriasis the earliest observable electron microscopic changes are in the papillary dermis vasculature. Selective photothermolysis of the dermal vasculature using a 585-nm pulsed-dye laser (PDL) for the treatment of psoriasis was reported more than a decade ago. Although clinically effective, the pulsed-dye laser has limited practicality because of small spot size (5-10 mm) and lack of cost effectiveness. The objective of this study is to evaluate the safety and efficacy of a novel Light and Heat Energy (LHE™) selective-photothermolysis system for the treatment of psoriasis. This system delivers controlled heat simultaneously with the light pulse; it has a large beam spot (55 × 22 mm) and is sufficiently cost effective to be widely used. Thirteen patients, seven with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis participated in a controlled study. Patients received two therapy regimens in parallel: LHE™ plus salicylic acid or salicylic-acid cream alone as control. Treatments were applied twice weekly spread evenly over 4-6 weeks. In most cases a fluence of 8.6 J/cm² was applied. Efficacy of the treatment was assessed using the psoriasis-severity index (PSI) calculated from the investigator's overall assessment of the plaque's erythema, scaling, and induration. PSI was evaluated at baseline, at every other treatment visit, and during two follow-up visits scheduled 1 and 5 weeks following the last treatment.
In eleven patients who completed the treatment regimen, the average global PSI score for the treated sites was reduced by 65 percent. In contrast, the control sites average global PSI score was reduced by only 7.4 percent. Six patients (55 %) had a significant improvement of 70-percent reduction or above in their PSI score, ten patients (91 %) had a 50 percent or above reduction; only one patient had a poor response (12.5 % reduction in global PSI). Erythema was reported in all cases and resolved within 24-48 hours. Six cases of burns were resolved within 2 days to 2 weeks following appropriate remedy. No cases of dyspigmentation were encountered.
Light and Heat Energy (LHE™) selective photothermolysis combined with salicylic acid appears to be a practical modality for the treatment of mild to moderate psoriasis. Patients experience discomfort that is only mild. There is no convalescence downtime. Clinical results obtained are similar to those reported with the pulsed-dye laser; however, this new system seems more suitable to be widely adopted as a treatment modality. Further followup is required to determine whether remission periods will be as long as those reported for treatment with the pulsed-dye laser.
Introduction
In psoriasis, the earliest observable electron-microscopic changes are in the papillary dermal vasculature. These vessels have been implicated as participating in the pathogenesis of the disease by facilitating the access of activated T cells to the skin and maintaining the psoriatic plaque [1, 2]. Treatment of psoriasis by selective photothermolysis of the dermal vasculature using a 585-nm pulsed-dye laser (PDL) has been suggested; several studies on the use of this laser to treat psoriasis have been published [3, 4, 5, 6, 7, 8]. Ros et al. [5] found a beneficial clinical effect on six of ten patients treated with PDL. The psoriasis-severity score in these patients was reduced to 2.2 ± 1.3, compared with 7.2 ± 1.7 for control areas (69 % reduction). Plaques readily developed crusting in which the necrotic former epidermis was apparent. Zelickson et al. [6] found significant clinical improvement in chronic plaque-type disease using both short (0.45 ms) and long (1.5 ms) pulsed-dye laser. Patients responding to treatment remained in remission for up to 13 months. A more recent followup found that some of the patients are still clear of the disease 5-6 years out. One patient showed no recurrence 7 years after PDL treatment. Although clinically effective, pulsed-dye laser has limited practicality because of a small (5-10 mm) spot size and lack of cost effectiveness.
The Radiancy Light and Heat Energy (LHE™) system is a new, potentially more effective selective-photothermolysis system for the treatment of psoriasis. In addition to green and yellow light for the coagulation of the psoriatic capillaries, this nonlaser system also emits a pulse of heat, which reduces swelling and inflammation and relieves pruritus [9, 10]. Using a broadband flashlamp, this small, tabletop device delivers a light energy fluence of 4-10 J/cm² with a beam spot of 55 × 22 mm, enabling rapid coverage of large lesion areas.
Methodology and treatment
A study was undertaken to assess the safety and efficacy of this LHE™ system in the treatment of patients with psoriasis. The study was designed as an intrapatient controlled study comparing the efficacy of two therapies for psoriasis given in parallel: LHE™ plus 20 percent salicylic acid (SCA) and 20 percent salicylic acid alone. The study was jointly conducted by the departments of plastic surgery and dermatology, Kaplan Hospital, Israel, following approval of the Helsinki Committee. Thirteen patients were enrolled in the study, seven with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis. Patients received two therapy regimens in parallel: ten biweekly treatments of LHE plus salicylic acid for a total of 5 weeks or salicylic-acid cream alone for the same time duration. In both regimens patients were asked to apply SCA daily except during treatment days. Treatment areas were a single (unilateral) plaque or double (bilateral), symmetrical plaques. In case of bilateral lesions, the right side was treated with LHE plus SCA; the left side was treated with SCA alone. In case of a unilateral lesion, the upper segment was treated with LHE plus SCA; the lower segment was treated with SCA alone.
Photographs of the psoriatic lesions were taken at baseline, at every other treatment visit, and during the first and second follow-up visits, conducted at 1 and 5 weeks following the last treatment.
Efficacy of the treatment was assessed using the Psoriasis Severity Index (PSI) calculated from the investigator's overall assessment of the plaque erythema, scaling, and induration. Score was defined as 0 = absent; 1 = minimal, light pink, rare scale, barely perceptible elevation; 2 = mild light red/pink, poorly defined scale, light elevation; 3 = moderate red, defined scales, moderate elevation; 4 = severe. very red, heavy scales, marked ridge. Global PSI score was calculated as the sum of erythema, scaling, and induration scores. PSI was evaluated at baseline, at every other treatment visit and during the first and second follow-up visits. The investigator performing the assessment was not blinded to treatment.
A total of thirteen patients with psoriasis were enrolled to the study in accordance with the following criteria:
- The patient is at least 18-years old.
- The patient has clinically diagnosed mild to moderate psoriasis (at least 10 % body area).
- Psoriasis is relatively symmetric and homogeneous.
- The patient is not on any other treatment.
- The patient is capable of reading, following instructions, and understanding the procedure to be applied.
- The patient is committed to all treatment and follow-up visits.
The patients were excluded according to the following criteria:
- The patient has used topical or systemic antipsoriatic therapy within 3 weeks prior to the start of the study.
- The patient has a history of carcinoma of the skin.
- The patient has used of any medication that can cause photosensitivity or affect integrity of the skin.
- The patient has had sun exposure or artificial tanning in the treatment area 2-weeks prior to study enrollment.
- The patient has a history of photosensitivity or intolerance to ultraviolet radiation.
The patient has a history of hypertrophic scar or keloid formation.
- The patient has a history of pigmentary changes in areas of trauma or burn.
- The patient has existing skin diseases other than psoriasis.
- The patient is pregnant
- The patient has epilepsy.
Before enrollment each patient completed a medical history form and signed an informed consent form. Three patients did not complete the treatment and followup for various reasons: One dropped out after the first visit, another after the third treatment, and the third completed treatments but did not appear for the follow-up visits. Mean age of the patients was 53.6 ± 6.4 years (range 44-67). Ten patients were females and three males. Six patients were Fitzpatrick skin types II (5 female, 1 male), five patients were skin types III (4 female, 1 male), and two were skin types V (1 female, 1 male).
Seven patients were diagnosed with plaque psoriasis, five with palmoplantar psoriasis, and one with guttate psoriasis. Three patients were treated on the elbow, two on the knee, one on the palm, five on the foot, three on the leg, and three on the arm.
Patients were instructed to clean the area thoroughly with soap and water and ensure that the skin surface is dry before treatment. On the basis of a pretreatment test conducted 48-72 hours prior, the highest power level that caused redness and erythema without blisters was used for treatment. Pulses were administered sequentially on the treatment area from right to left with no more than 20 percent overlap. After covering the entire area the investigator waited 5 minutes to allow the skin to cool, and repeated the procedure once more. For small lesions, a small-area adaptor was used. In this case fluence was increased by 10 percent to compensate for light scatter. Treatments were applied twice weekly spread evenly over a 4-6 week period. When no results were seen after 3 treatments, fluence was increased by 10 percent.
In most cases a fluence of 8.6 J/cm² was found to be the most effective and safe treatment parameter.
Results
Plaque assessment on the treated site (LHE plus SCA) and the control site (SCA alone) was conducted by the investigator at baseline, prior to any treatment, at each odd-numbered treatment visit and at the two follow-up visits. Of the eleven patients who completed the treatment regimen, one underwent a total of 8 treatments, three a total of 10 treatments, three a total of 11 treatments, and four a total of 12 treatments.
Figure 1
Average global PSI at different stages of treatment.
Average global PSI score at baseline for the treated sites (LHE plus SCA) was 8.36 (range 6-11). This was reduced by 65 percent to 2.91 (range 0-7) at the final visit. Scaling score in these sites was reduced from an average of 2.82 to 1.00 (64 % reduction); erythema score was reduced from 2.64 to 1.00 (62 %); and induration score was reduced from 2.91 to 0.91 (69 %). Nine patients appeared for the first follow-up visit (FU1), and only seven for the second follow-up visit (FU2). In this latter group, average global PSI score further reduced to 2.57 (69 %) possibly indicating the effect of the final treatment. The reduction in global PSI score, over the treatment course, for the lesions treated with LHE plus SCA is shown in Fig. 1.
Of the eleven patients who completed the treatment regimen only one had a poor response (12.5 % reduction in global PSI). Ten of the patients (91 %) had a 50 percent or above reduction in their PSI score, and six patients (55 %) had a significant improvement of 70 percent reduction or above.
In contrast, on the control sites (SCA alone) average global PSI score at baseline was 7.71 (range 4-10), and this score was reduced by only 7.4 percent to an average of 7.14 (range 3-9). Scaling was reduced by 5.2 percent, erythema by 5.8 percent, and induration by 10.9 percent.
Figure 2a
Figure 2b
Before treatment (Fig. 2). After treatment (Fig. 2a).
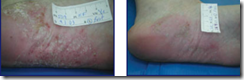
Figure 3a
Figure 3b
Before treatment (Fig. 3). After treatment (Fig. 3a).
Figure 4a
Figure 4b
Before treatment (Fig. 4). After treatment (Fig. 4a).
Figure 5a
Figure 5b
Before treatment (Fig. 5). After treatment (Fig. 5a).
The safety of the LHE psoriasis treatment was determined by clinical observation and evaluation of the treated areas. Potential adverse clinical effects, such as erythema, crusting, blistering, scars, and hyper- or hypopigmentation, were evaluated by the investigator in each treated area immediately after treatment, between treatments, and during the follow-up visits. Erythema was reported in all cases and resolved within 24-48 hours. Six cases of burns (five with blistering) were reported; these patients were given appropriate remedy (Silverol or Biafine) and the reaction resolved within 2 days to 2 weeks. No cases of dyspigmentation were encountered.
Conclusions
Radiancy's Light and Heat Energy (LHE™) selective-photothermolysis system, combined with salicylic acid, appears to be an effective modality for the treatment of mild to moderate psoriasis. In most cases (6/10) a significant reduction of over 70 percent in global PSI score was achieved. In almost all cases (10/11) at least a moderate improvement (greater than 50 %) was obtained; only one case resulted in insignificant (12.5 % reduction) response. Overall, average global PSI score for the eleven patients who completed the treatment regimen was reduced by 65 percent from 8.36 to 2.91. In contrast, control treatment of salicylic acid alone resulted in an average global PSI score reduction of only 7.4 percent. No improvement occurred in 71 percent of the control lesions, and 29 percent exhibited very modest improvement.
Side effects were mild and transient with resolution at 2 weeks post-treatment at most. The only discomfort patients experienced was mild. There was no downtime for convalescence.
The clinical results obtained with the Radiancy LHE™ system in the treatment of psoriasis are remarkably similar to those reported with the pulsed-dye laser. In contrast to pulsed-dye laser, the LHE system is compact, simple to operate, and cost effective; we consider this form of treatment to be highly suitable to be widely adopted as a treatment modality for mild to moderate psoriasis. Further followup is required to determine whether remission periods will be as long as those reported for treatment with the pulsed-dye laser.
Conflict of Interest Statement: A Vilan is a medical consultant for Radiancy. Drs. Leviav and Wolf have no financial interest relating to this work.
References
1. Pinkus H, Mehregan AH. The primary histologic lesion of seborrhoic dermatitis and psoriasis. J Invest Dermatol. 46:109-116, 1966.2. Barker JN. The pathophysiology of psoriasis. Lancet. 1991 Jul 27;338(8761):227-30. PubMed
3. Hacker SM, Rasmussen JE. The effect of flash lamp-pulsed-dye laser on psoriasis. Arch Dermatol. 1992 Jun;128(6):853-5. PubMed
4. Katugampola GA, Rees AM, Laningan SW. Laser treatment of psoriasis. Br J Dermatol. 1995 Dec;133(6):909-13. PubMed
5. Ros AM, Garden JM, Bakus AD, Hedblad MA. Psoriasis response to the pulsed-dye laser. Lasers Surg Med. 1996;19(3):331-5. PubMed
6. Zelickson BD, Mehregan DA, Wendelschfer-Crabb G, Ruppman D, Cook A, O'Connell P, Kennedy WR. Clinical and histologic evaluation of psoriatic plaques treated with a flashlamp pulsed-dye laser. J Am Acad Dermatol. 1996 Jul;35(1):64-8. PubMed
7. Bjerring P, Zachariae H, Sogaard H. The flashlamp-pumped dye laser and dermabrasion in psoriasis--further studies on the reversed Kobner phenomenon. Acta Derm Venereol. 1997 Jan;77(1):59-61. PubMed
8. Hern S, Allen MH, Sousa AR, Harland CC, Barker JN, Levick JR, Mortimer PS. Immunohistochemical evaluation of psoriatic plaques following selective photothermolysis of the superficial capillaries. Br J Dermatol. 2001 Jul;145(1):45-53. PubMed
9. Orenberg EK, Noodleman FR, Koperski JA, Pounds D, Farber EM. Comparison of heat delivery systems for hyperthermia treatment of psoriasis. Int J Hyperthermia. 1986 Jul-Sep;2(3):231-41. PubMed
10. Boreham DR, Gasmann HC, Mitchel RE. Water bath hyperthermia is a simple therapy for psoriasis and also stimulates skin tanning in response to sunlight. Int J Hyperthermia. 1995 Nov-Dec;11(6):745-54. PubMed





No comments:
Post a Comment